Transition to palliative care
facilitating actions for cancer client-centered communication
DOI:
https://doi.org/10.5935/1415.2762.20200070Keywords:
Medical Oncology, Communication, Palliative CareAbstract
Introduction: the professional-client interpersonal relationship becomes fundamental in the transition to palliative care so that together they can improve communication at that time and align care to the client's wishes. Objective: to analyze how the cancer client evaluates communication in the transition to palliative care; identify your needs and preferences regarding
this communication related to your prognosis, decision making and family participation; and present a proposal for facilitating actions for communication in the transition to palliative care, based on the needs and preferences mentioned by the client. Method: convergent care research conducted at a federal hospital in Rio de Janeiro, with 15 cancer patients. A semi-structured interview was used,
followed by a dialogue with each participant. Thematic analysis applied. Results: in the evaluation of the participants, the welcoming, the attentive way, the truth
information and the simple and accessible language were essential elements to build a relationship of trust and enlightening communication about the moment lived. Still, clients were looking forward to more information about their treatment and prognosis. Although the majority mentioned the preference for the truth, family
participation and active participation in the treatment, others demonstrated the preference for not knowing in order not to suffer, non-family participation and passivity in the participation in the treatment. Conclusion: it will be from the prioritization of active listening actions, welcoming, respect for autonomy and the use of clear and accessible language that the professional will create the necessary bond and be more successful in carrying out a communication centered on the needs and preferences of the cancer client.
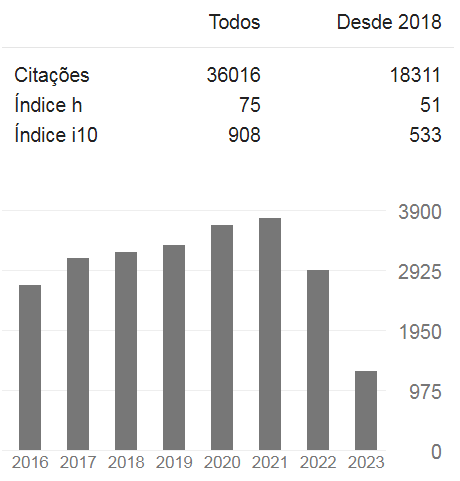
Downloads
References
Sawada NO, Paiva BSR, Paiva CE, Sonobe HM, García-Caro MP, Cruz-Quintana F. Abordagem transcultural da qualidade de vida relacionada à saúde de pacientes com câncer. Rev Rene. 2017[citado em 2020 abr. 01];18(3):368-75. Disponível em: http://dx.doi.org/10.15253/2175-6783.2017000300012
Silva CP, Santos ATC, Silva RP, Andrade JD, Almeida LM. Significado dos cuidados paliativos para a qualidade da sobrevivência do paciente oncológico. Rev Bras Cancerol. 2016[citado em 2020 jul. 31];62(3):225-35. Disponível em: https://doi.org/10.32635/2176-9745.RBC.2016v62n3.164
World Wide Palliative Care Alliance. Global atlas of palliative care at the end of life. London: WHO; 2014.
Andrade CG, Costa SFG, Lopes MEL. Cuidados paliativos: a comunicação como estratégia de cuidado para o paciente em fase terminal. Ciênc Saúde Colet. 2013[citado em 2020 abr. 01];18(9):2523-30. Disponível em: https://dx.doi.org/10.1590/S1413-81232013000900006
Santos FS. Cuidados paliativos: discutindo a vida, morte e o morrer. Rio de Janeiro: Atheneu; 2016.
Silva MJP, Araújo MMT. Comunicação em cuidados paliativos. In: Carvalho RT, Parsons HA. Manual de cuidados paliativos ANCP. 2ª ed. São Paulo: ANCP; 2012. 75-85p.
Almeida KLS, Garcia DM. Use of communication strategies in palliative care in Brazil: integrative review. Cogitare Enferm. 2015[citado em 2020 abr. 01];20(4):720-7. Disponível em: http://dx.doi.org/10.5380/ce.v20i4.39509
Borges MM, Santos Junior R. A comunicação na transição para os cuidados paliativos: artigo de revisão. Rev Bras Educ Méd. 2014[citado em 2020 jul. 31];38(2):275-82. Disponível em: http://dx.doi.org/10.1590/S0100-55022014000200015
Brighton LJ, Bristowe K. Communication in palliative care: talking about the end of life, before the end of life. Postgrad Med J. 2016[citado em 2020 abr. 01];92(1090):466-70. Disponível em: http://dx.doi.org/10.1136/postgradmedj-2015-133368
Galvão MIZ. Comunicação interpessoal em cuidados paliativos: um estudo à luz da teoria de Peplau [dissertação]. Brasília (BR): Universidade de Brasília; 2016.
Peplau HE. Interpersonal relations in nursing: a conceptual frame of reference for psychodynamic nursing. New York: Springer Publishing; 1991.
Trentini M, Paim L, Silva DMGV. Pesquisa convergente-assistencial: delineamento provocador de mudanças nas práticas de saúde. 3ª ed. Porto Alegre: Moriá Editora; 2014.
Freire MSS, Nery IS, Silva GRF, Luz MHB, Rodrigues IDCV, Santos LNM. Nursing care for women with breast cancer based on the theory of interpersonal relations. Rev Enferm UFPE on line. 2013[citado em 2020 abr. 01];7(esp):7209-14. Disponível em http://dx.doi.org/10.5205/reuol.4767-42136-1-ED.0712esp201333
Santos LNM, Pedrosa JIS, Rodrigues IDCV, Freire MSS, Silva GRF, Luz MHBA. Interpersonal relations in the family health strategy: effects on nursing care quality. Rev Enferm UFPE on line. 2014[citado em 2020 abr. 01];8(1):155-9. Disponível em: http://dx.doi.org/10.5205/reuol.4843-39594-1-SM.0801201421
Minayo MCS, Deslandes SF, Gomes RC. Pesquisa social: teoria, método e criatividade. Petrópolis: Vozes; 2015.
Stefanelli MC, Carvalho EC. A comunicação nos diferentes contextos da Enfermagem. Barueri: Manole; 2012.
Gomes ALZ, Othero MB. Cuidados paliativos. Estud Av. 2016[citado em 2020 abr. 01];30(88):155-6. Disponível em: http://dx.doi.org/10.1590/S0103-40142016.30880011
Caponero R. A comunicação médico-paciente no tratamento oncológico: um guia para profissionais de saúde, portadores de câncer e seus familiares. São Paulo: MG Editores; 2015.
Abreu CBB, Fortes PAC. Questões éticas referentes às preferências do paciente em cuidados paliativos. Rev Bioét. 2014[citado em 2020 abr. 01];22(2):299-308. Disponível em: https://dx.doi.org/10.1590/1983-80422014222011
Carey M, Lambert S, Smits R, Paul C, Sanson-Fisher R, Clinton-Mcharg T. The unfulfilled promise: a systematic review of interventions to reduce the unmet supportive care needs of cancer patients. Support Care Cancer. 2012[citado em 2020 abr. 01];20(2)207-19. Disponível em: http://dx.doi.org/10.1007/s00520-011-1327-1
Coelho CBT, Yankaskas JR. New concepts in palliative care in the intensive care unit. Rev Bras Ter Intensiva. 2017[citado em 2020 abr. 01];29(2):222-30. Disponível em: http://dx.doi.org/10.5935/0103-507x.20170031
Oostendorp LJM, Ottevanger PB, Van de Wouw AJ, Honkoop AH, Los M, Van der Graaf WT, et al. Patients’ preferences for information about the benefits and risks of second-line palliative chemotherapy and their oncologist’s awareness of these preferences. J Cancer Educ. 2016[citado em 2020 abr. 01];31(3):443-8. Disponível em: http://dx.doi.org/10.1007/s13187-015-0845-9
Brom L, Pasman HR, Widdershoven GA, Van der Vorst MJDL, Reijneveld JC, Postma TJ et al. Patients’ preferences for participation in treatment decisionmaking at the end of life: qualitative interviews with advanced cancer patients. PLos ONE. 2014[citado em 2020 abr. 01];9(6):e100435. Disponível em: http://dx.doi.org/10.1371/journal.pone.0100435
Pessini L. Bioética e cuidados paliativos. In: Pimenta CAM, Mota DDCF, Cruz DALM. Dor e cuidados paliativos: Enfermagem, medicina e psicologia. Barueri: Manole; 2006. p.45-66.
Öhlén J, Carlsson G, Jepsen A, Lindberg I, Friberg F. Enabling sense-making for patients receiving outpatient palliative treatment: a participatory action research driven model for person-centered communication. Palliat Support Care. 2016[citado em 2020 abr. 01];14(3):212-24. Disponível em: https://dx.doi.org/10.1017/S1478951515000814
Published
How to Cite
Issue
Section
License
Copyright (c) 2020 Reme: Revista Mineira de Enfermagem

This work is licensed under a Creative Commons Attribution 4.0 International License.