Planejamento estratégico em saúde no Brasil:
ascensão e desprestigio
DOI:
https://doi.org/10.35699/2316-9389.2024.49473Palavras-chave:
Planejamento em Saúde, Planejamento Estratégico, Planejamento normativo, Administração em Saúde, Comunicação em Saúde, Políticas, Planejamento e Administração em SaúdeResumo
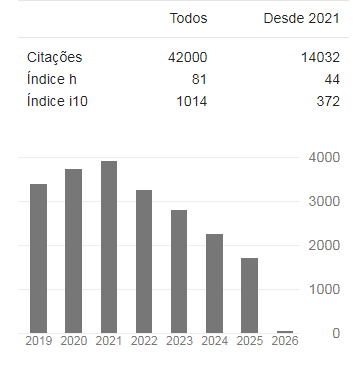
Este estudo é de caráter reflexivo e tem como objetivo revisitar conceitos e marcos históricos do planejamento em saúde no Brasil, refletindo sobre sua ascensão e subsequente desprestígio. O Planejamento em Saúde na América Latina surgiu inspirado pela racionalidade econômica, tendo como modelo o Método CENDES/OPAS, buscando alcançar melhores resultados. No Brasil, na década de 60, o planejamento normativo utilizou a programação centralizada para responder a problemas prioritários. Como resposta à ditadura e à crise econômica, o Planejamento Estratégico (PE) começou a ser visto como uma alternativa eficaz ao normativo, com o intuito de estabelecer novas formas democráticas e participativas de planejar as instituições. Mario Testa abordava o PE na perspectiva da transformação e construção histórica de uma nova sociedade. Carlos Matus destacava a análise situacional como ferramenta fundamental para a governabilidade e melhoria nas respostas e capacidade de governo. A análise institucional buscou novos arranjos institucionais, visando ampliar o diálogo e criar corresponsabilidades entre os indivíduos no processo de transformação e democratização da organização. Entre os anos 80 e 2000, esses métodos foram amplamente utilizados nos currículos de graduação, pós-graduação e serviços. Os métodos e instrumentos do PE foram importantes na implantação do SUS e na promoção de sociedades mais democráticas e participativas, revelando sua ascensão e prestígio. Progressivamente, o instrumental do PE foi substituído pela ênfase no desempenho e no gerencialismo, com o progressivo abandono das análises de contextos e políticas, caracterizando seu declínio, o que pode ser mensurado na academia pela redução das publicações, pesquisas e ensino sobre a temática.
Downloads
Referências
1. Romo CM. Adeus senhor presidente: governantes e governados. São Paulo: Edições FUNDAP; 1997.
2. Merhy EE. Planejamento como tecnologia de gestão: tendências e debates no planejamento em saúde no Brasil. In: Gallo E. Razão e planejamento: reflexões sobre política estratégia e liberdade. São Paulo: Hucitec; Rio de Janeiro: Abrasco; 1995.
3. Furtado JP, Campos GWS, Oda WY, Onocko-Campos R. Planejamento e avaliação em saúde: entre antagonismo e colaboração. Cad Saúde Pública [Internet]. 2018[citado em 2024 jan. 08];34(7): e00087917. Disponível em: https://doi.org/10.1590/0102-311X00087917
4. Fekete MC. Planejamento e programação em saúde: bases conceituais e metodológicas do planejamento em saúde. In: Ministério da Saúde (BR). Gestão municipal de saúde. Brasília: Ministério da Saúde; 2001. p. 201-17.
5. Gentilini JA. Atores, cenários e planos: o planejamento estratégico situacional e a educação. Cad Pesqui [Internet]. 2014[citado em 2024 jan. 08];44(153):580-601. Disponível em:
https://doi.org/10.1590/198053142954
6. Rivera FJU. Planejamento e programação em saúde: um enfoque estratégico. São Paulo: Cortez; 1989.
7. Giovanella L. Planejamento estratégico em saúde: uma discussão da abordagem de Mário Testa. Cad Saúde Pública [Internet].1990 [citado em 2024 jan. 08];6(2):129-53. Disponível em: https://doi.org/10.1590/S0102-311X1990000200003
8. Merhy EE. Saúde: a cartografia do trabalho vivo. São Paulo: Hucitec; 2007.
9. Testa M. Estrategia, coherencia y poder en las propuestas de salud. Cuad Med Soc (Ros.) [Internet].1987[citado em 2024 jan. 08];38(4 Pt 1):24. Disponível em: https://web.amr.org.ar/cuadernos-medicos-sociales/
10. Mattos RA. (Re)visitando alguns elementos do enfoque situacional: um exame crítico de algumas das contribuições de Carlos Matus. Cien Saude Colet [Internet]. 2010[citado em 2024 jan. 08];15(5):2327-36. Disponivel em: https://doi.org/10.1590/S1413-81232010000500008
11. Merhy EE, Onoko R. Agir em saúde: um desafio para o público. São Paulo: Hucitec; 1997.
12. Habermas J. Éthique de la discussion. Paris: Cerf; 1992.
13. Baremblit G. Compêndio de análise institucional. 3a ed. Rio de Janeiro: Rosa dos Tempos; 1996.
14. Malta DC, Merhy EE. A micropolítica do processo de trabalho em saúde, revendo alguns conceitos. REME Rev Min Enferm [Internet]. 2003[citado em 2024 jan. 08];7(1):61-6. Disponível em: https://periodicos.ufmg.br/index.php/reme/article/ view/50937
15. Zaffaroni C. El marco de desarrollo de base: la construcción de un sistema participativo para analizar resultados de proyectos sociales. Montevideo: Trilce; 1997.
Arquivos adicionais
Publicado
Edição
Seção
Licença
Copyright (c) 2025 REME-Revista Mineira de Enfermagem

Este trabalho está licenciado sob uma licença Creative Commons Attribution 4.0 International License.